Eliad Josephson, Subject Matter Expert - Diagnostics @ HLTH
Diagnostics are enabling a world where clinicians can detect disease before symptoms appear, where care is personalized based on an individual’s molecular profile, and where remote diagnostics bring health access to every corner of society.
That world isn’t far, it's unfolding now: transforming not just how we treat disease, but how patients experience care through faster diagnoses, more targeted therapies, fewer complications, and earlier interventions that reduce long-term costs.
Diagnostics have always been the bedrock of medicine, guiding therapy, informing prognosis, and ensuring prudent use of resources.
As we move from centralized labs to living rooms, diagnostics are no longer just tools - they’re the catalyst transforming how we understand, deliver, and democratize healthcare.
The Status Quo: Underfunded, Overrelied On
Diagnostics play a bigger role in healthcare than most people realize.They shape approximately 70 % of clinical decisions worldwide, but receive only 3–5 % of healthcare budgets (based on a recent report from the World Health Organization)
Think about that: the backbone of medical decision-making remains vastly under-resourced.
Bridging this investment gap isn’t just smart economics; it enables earlier treatment, reduces costly downstream interventions, and drives better long-term health outcomes for patients.
Scaling to Billions: Exponential Market Growth
The global clinical diagnostics market is poised to grow from $82.6B in 2024 to nearly $147.2B by 2035 (5.5 % CAGR) -
The laboratory diagnostics segment alone was valued at $60B in 2024 and is projected to reach $95B by 2033 (5.1 % CAGR) -
Next-gen IVDs (genomics, proteomics, molecular assays) stand at $9.7B in 2025, driven to $15.6B by 2034.
Point‑of‑care (POC) diagnostics, devices and tests used at the bedside, in clinics, or at home, are accelerating: from $62.3B in 2024 to $82.8B by 2034 (~2.9 % CAGR).
In the U.S. alone, diagnostic testing soared to $84.9B in 2023, framed to hit $158.8B by 2033 (~6.5 % CAGR).
Behind these numbers is a story of better resource use: catching disease earlier, avoiding unnecessary admissions, and enabling more efficient, value-based care.
Why Now—And Why This Matters (Who Cares? As Steve Jobs would say)
1. Disease Burden & Preventive Care
As chronic illnesses surge from diabetes and heart disease to various cancers, early detection becomes increasingly vital.
Funders and policymakers now understand that diagnostics are preventive, not just reactive.
For example, a recent study analyzed data from over 400,000 individuals. It found that polygenic risk scores (genetic screening tools) can identify individuals who reach high-risk thresholds 12.4 years earlier than typical screening protocols. Implementing these tools could prevent 24.5% of premature deaths from common conditions like breast cancer, diabetes, hypertension, and cardiovascular disease.
An OECD working paper from early 2025 highlighted that halving diagnostic errors and standardizing diagnostic practices could save up to 8% of total healthcare spending in OECD countries. That is nearly 1.8% of GDP per country. In the U.S., diagnostic errors are estimated to affect 12 million people annually (nearly 1 in 20 adults) demonstrating both the clinical urgency and economic scale of the problem.
The health and economic value is real: reduced emergency room visits, avoided hospitalizations, and longer disease-free lives. Preventive diagnostics shift the curve from crisis care to sustainable, proactive management.
2. Molecular & Omics Revolution
We’re entering an era of precision diagnostics, where disease is decoded at the genetic, transcriptomic, proteomic, and even microbiomic levels.
Sequencing-driven tools, from NGS‑based cancer panels to pharmacogenomic tests, empower practitioners to tailor treatments, raising efficacy while minimizing collateral impacts.
For patients, this leads to fewer adverse events, more effective care, and reduced trial and error prescribing. This translates to improved quality of life and fewer system costs.
However, coverage gaps, limited clinical integration, and high upfront costs still restrict access, especially outside urban health systems.
3. AI & Big Data Integration
The convergence of AI, machine learning, and big healthcare data is revolutionizing diagnostics. AI streamlines imaging workflows, detects anomalies in radiology faster, and interprets genetic data with greater precision.
Consider:
The FDA’s recent approvals of AI systems for skin cancer, prostate, and breast cancer detection.
Intel giants like NVIDIA and Microsoft are partnering to integrate AI into medical imaging analysis, promising early detection and cost reduction.
In the lab, AI is also helping automate high-volume workflows, optimizing throughput, reducing manual steps, and alleviating staffing shortages.
AI doesn't replace expert judgment. It enhances it. By offering faster pattern recognition and richer insights, it equips healthcare professionals to make better-informed decisions.
This leads to faster diagnosis, reduced human error, and more efficient care coordination. All of which reduce time to treatment and cost of care.
Still, clinicians need better tools for trust building, explainability, and validation across diverse populations.
4. Decentralized & Point‑of‑Care Access
Diagnostic decentralization is reshaping care paradigms today.
POC testing brings immediate results to community clinics and homes, erasing friction in rural or underserved environments. Recently, new federal legislation allocated $50 billion in funding to support rural hospitals and expand healthcare access in underserved communities.
Kits for glucose monitoring, infectious diseases, and heart markers allow clinicians and patients alike to act in real time.
Self-collection methods and non-invasive alternatives are also reducing barriers tied to geography, stigma, and comfort. Bringing diagnostics physically and emotionally closer to patients.
Even wearable sensors and digital diagnostics are gaining momentum.
As IQVIA’s 2024 report noted, provider-focused digital diagnostic platforms linked to decision support and remote monitoring are improving chronic disease outcomes worldwide. The result? Shorter time to diagnosis, lower system utilization, and empowered patient self management.
But achieving widespread coverage and reimbursement for home based and remote diagnostics remains a major hurdle.
5. Coordinated Diagnostics for System Efficiency
“Coordinated diagnostics” is emerging as a holistic model, interlinking labs, imaging centers, EHR systems, payers, and patients for real-time, optimized decision-making.
This supports smarter, value-based care, reducing over-testing, streamlining workflows, and lowering costs. This not only reduces waste. It improves continuity of care and lowers diagnostic error, especially for complex conditions. Digital diagnostics reduce administrative burden, speed up billing cycles, and improve lab profitability. This is potentially translating efficiency into economic value for health systems.
But fragmented infrastructure and non standardized data formats still limit true interoperability.
Real‑World Innovation Spotlight
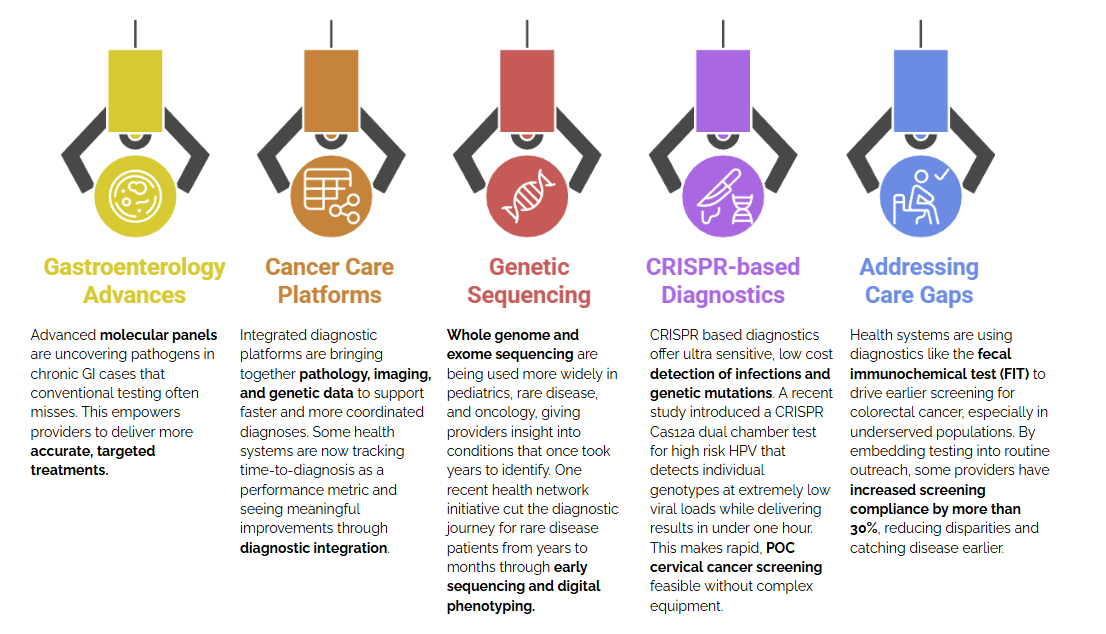
These innovations show a broader truth: diagnostics aren’t just measuring health. They are driving smarter, faster, and more equitable care across the entire system.
The Imperatives for Health Systems
Invest Strategically
Diagnostics represent high ROI: improved outcomes, shorter hospital stays, and reduced downstream costs. Redirecting even 1 – 2 % of healthcare budgets into diagnostics could yield outsized system benefits.Champion Equity & Access
True impact depends on democratizing diagnostics and ensuring innovations reach rural, low‑resource, and marginalized communities. Support for POC platforms, telehealth links, and training is essential.Foster Interoperability
Data-sharing across systems, labs, and platforms (while protecting patient privacy) is critical. AI accuracy depends on diverse, robust datasets and real-world validation.Modernize Regulation
Agile regulatory frameworks that embrace AI and molecular tools without compromising safety can accelerate delivery into clinical practice.Educate & Engage Clinicians
Tools don’t change outcomes. People do. Comprehensive clinician education, trust-building, and responsible implementation designs are key enablers.
Diagnostics as the Heartbeat of Tomorrow’s Healthcare
From foundational lab tests to AI-enhanced genomic diagnostics and universal digital platforms, diagnostics is the beating heart of modern care.
As markets surge, technologies pulse with innovation, and real-world deployments gain traction, we stand at a pivotal moment. Healthcare is evolving from reactive to predictive, from generic to personalized, and from siloed to connected.
For patients, this means better outcomes with less friction: fewer unnecessary procedures, more effective treatments, and earlier detection of disease when it’s still manageable or even preventable.
It’s time for healthcare leaders to treat diagnostics not as a cost center, but as a strategic asset that advances precision, equity, and system resilience.
Diagnostics is driving the future of healthcare - faster, smarter, and more personalized.
At HLTH USA 2025, we’re spotlighting the breakthroughs redefining early detection, precision medicine, and system-wide efficiency. From genomics to digital pathology, join the leaders turning science into scalable, life-changing solutions.
👉 Be a part of the diagnostics transformation at HLTH USA 2025
