In an industry saturated with hype and "next big thing" fatigue, the HLTH Insights Council (US) serves as the definitive filter. We are proud to introduce this invitation-only collective of senior leaders across payers, providers, life sciences, and technology who serve as the architects of the HLTH 2026 year-round programming agenda. Meet the leaders directing this year's agenda and explore the critical insights from their inaugural meeting. Read on!
The HLTH Insights Council (US): 2026 Leadership
The Inaugural Meeting: Key Takeaways & Strategic Shifts
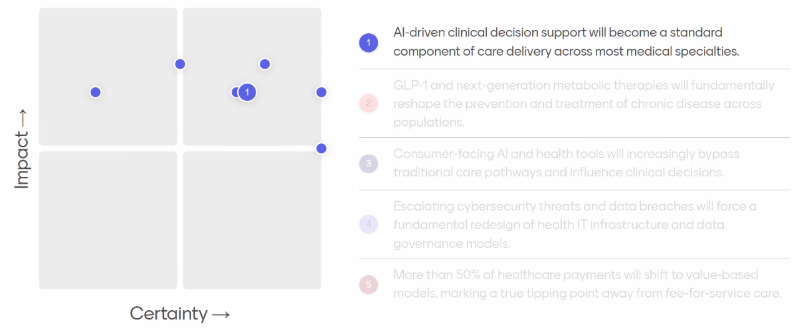
So what surfaced when the votes came in?
AI Is Moving Into Care - But Workflow, Not Capability, Determines Adoption
AI-driven clinical decision support will become a standard component of care delivery across most medical specialties.
Most of the Insights Council believe clinical decision support is moving forward, but there was a debate on how fast and how broadly it becomes standard practice.
The key distinction was between decision support and decision making.
When AI augments clinicians - embedded into workflows, operating in the background, and trusted as assistive infrastructure - adoption feels achievable. When it crosses into autonomous decision-making, concerns about validation, accountability, and safety rise quickly.
As one Council member put it:
“When AI is integrated directly into workflows, and trusted, it can meaningfully change behavior. Workflow, more than technology, is what drives adoption.”
That view was reinforced by on-the-ground behavior. Providers are already using AI tools informally at the point of care, creating pull for more formal integration. As another member noted:
“Providers are already using AI tools informally at the point of care. That openness will likely accelerate adoption once these tools are formally embedded into systems.”
Still, others grounded the discussion in operational reality:
“85% accuracy is insufficient in healthcare. If the data sets are not complete or if you have a gap in your information, the model will generate something and it may or may not be right.”
The implication was shared across the group: progress is no longer gated by model capability alone, but by data readiness, governance, and workflow integration - the slowest parts of the system.
The Bottleneck Has Shifted: From Building AI to Knowing What to Build
One of the clearest shifts surfaced in how leaders think about AI development itself.
For years, the hardest part of health technology was operationalization. In this meeting, it was argued that the challenge has moved upstream - to problem definition.
One member described the inversion succinctly:
“The hardest part now isn’t building AI solutions -it’s knowing what to build. Clarifying the problem and visualizing what’s possible have become more difficult than operationalizing the technology.”
AI lowers the cost of experimentation, but raises the bar on leadership judgment. Without clarity on outcomes, organizations risk deploying tools that work technically but fail strategically.
This reframing also fueled a broader theme: AI fluency. If AI is to be embedded across care, organizations need fluency not only among technologists, but among clinicians, operators, and leaders making prioritization decisions.
Consumer AI Is Inevitable - Stewardship Is Not Optional
If clinical AI prompted debate, consumer-facing AI prompted resignation.
On the statement that consumer AI and health tools will increasingly bypass traditional care pathways, the room largely agreed on direction - even if it diverged on impact.
As one member put it bluntly:
“Whether we like it or not, there is no escaping the inevitable that people will engage with these consumer-facing tools directly.”
Another member tied that inevitability to access gaps:
“We have a large number of people that will go uninsured, and that number is only increasing. People who don't have access to timely healthcare will shift to AI tools if they're getting value.”
Yet inevitability did not translate to optimism. The group returned repeatedly to trust, misinformation, and responsibility. As one member cautioned:
“I saw how pre-AI influencer culture eroded what should have been a heroic story of the vaccine being developed. There is less and less trust of experts.”
In that environment, clinicians and health systems face a new role.
“As clinicians, one of our emerging roles will be stewardship -helping patients navigate which tools and information sources are credible as choice expands.”
Consumer AI may not be optional - but guidance, oversight, and post-implementation monitoring are.
Cybersecurity: Everyone Agrees It Should Force Redesign - Fewer Believe It Will
On cybersecurity, the group drew a line between necessity and feasibility.
Most participants agreed that escalating threats should force a fundamental redesign of health IT infrastructure. Far fewer believed systems could realistically prioritize that work amid financial strain.
The dilemma was framed clearly in discussion: organizations know what needs to happen, but many are operating in survival mode - especially in rural and underserved settings. The result is a widening gap between “should” and “will,” with equity implications baked in.
Value-Based Care: When Progress on Paper Doesn’t Feel Like Progress in Practice
The most scattered chart of the session belonged to value-based care.
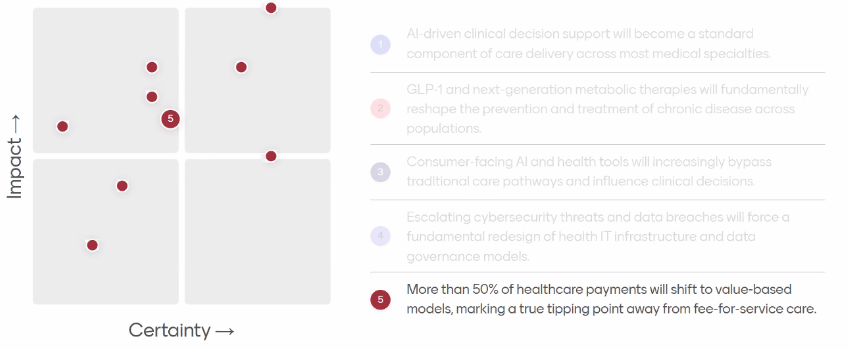
Some participants believed the system will reach the “50% of payments” threshold. Others doubted it would happen soon - or matter when it does.
The disagreement wasn’t about intent. It was about meaning.
One member voiced skepticism rooted in experience: incentives have shifted repeatedly, yet frontline behavior remains stubbornly fee-for-service. Another captured this nuance:
“You could easily draw a circle around and say yes, 50% will hit that threshold… But whether that has an impact is an open question. Meaningful value-based care? I’d be hesitant to speak strongly on that.”
The scatterplot made visible what many leaders feel privately: definition creep can create the appearance of progress without delivering structural change.
What HLTH Takes Forward
The Council's first meeting surfaced several themes that will directly shape HLTH Member programming. AI implementation is moving from capability questions to organizational readiness questions - around data quality, workforce fluency, and system redesign. Consumer-facing health tools are bypassing traditional pathways faster than infrastructure can adapt, raising urgent questions about stewardship and trust. Finally, investment is cooling in previously hot sectors while consolidating around practical problems like supply chain optimization and clinical trial efficiency. These are the realities HLTH members are working through right now.
For our Q2 and Q3 programming, this means focusing content on implementation gaps rather than technology potential, addressing how organizations build AI fluency at scale, exploring emerging payment models that actually incentivize prevention, and creating space for honest conversations about where innovation is stalling and why. The Council identified specific questions that need more attention: how systems act on what AI surfaces when capacity is limited, how clinicians guide patients through expanding consumer health tools, and whether value-based care definitions are expanding faster than meaningful change.
The Council will be in continued discussion, and reconvene in person later this year, with ongoing discussions shaping our virtual programming, Executive Masterclasses, and in-person member events throughout 2026 and beyond.